|
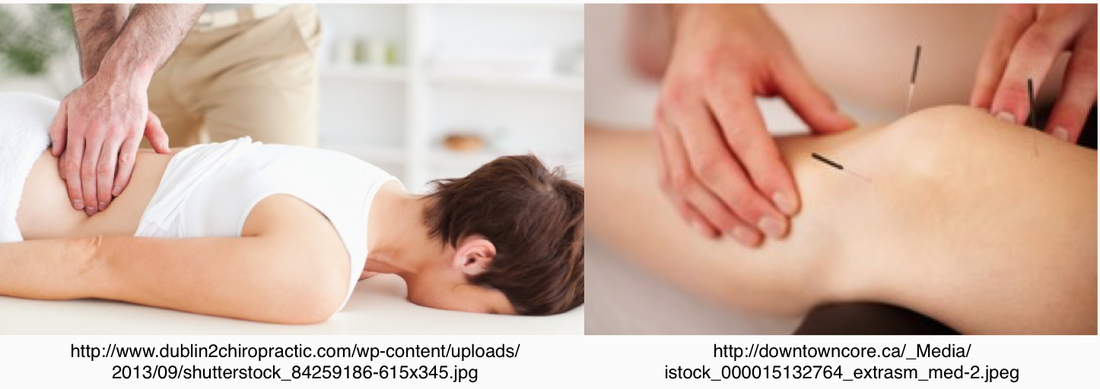
Chiropractic and acupuncture treatments can work together synergistically to treat a variety of symptoms and conditions. While the two treatments differ in their modalities, they both are non-invasive, drug free, non-surgical treatments designed to heal the body. Chiropractors help to fix the mechanisms of injury through adjustments and manipulations while acupuncturists help to promote the bodies natural healing processes. Both treatments are considered safe and healthy by researchers and health care professionals.
Acupuncture treatments focus on the regulation of the vital flow of qi, or energy, in the body by the precise insertion of thin metallic needles into the skin. One of the tenants of Chinese Medicine is that energy flows through your body in pathways called meridians. These pathways can become blocked, restricting the flow of qi which can result in an imbalance in the body. It is the insertion of these needles that break up and prevent the blocking of qi. Despite the uncomfortable image of having needles placed into you, the needles, when applied correctly, cause no pain. Rather, the sensation of the needle application is often described as a slight pinch or pressure. Acupuncture treatment can be used to correct this imbalance, and also for pain management, strengthening the immune system, improve respiratory health, relieve insomnia and reduce stress levels. Patients can benefit greatly from receiving treatment from an acupuncturist prior to visiting a chiropractor. Acupuncture treatments help to promote the release of endorphins and bodies natural healing mechanisms, reducing pain levels, inflammation and increases the blood flow to afflicted areas. This can help chiropractors conduct both spinal and joint readjustments and manipulation more easily, as the muscles around the afflicted areas are loose and not guarding injuries. In turn, chiropractors can help with a different method of the regulation of flow in the body. The spine is the main conduit for electrical impulse flow, sending signals from the brain throughout the body and sending bodily feedback back to the brain. Misaligned vertebrae, muscle tension or spinal injury can lead to improper function of the body due to blocked nerve impulses. Chiropractors perform readjustments and manipulations in order to restore and regulate this function. Combined, acupuncture and chiropractic treatment are a powerful holistic medicine duo that can treat patients healthily and safely. References: DrDuongLive: http://drduonglive.com/benefits-of-combining-chiropractic-care-and-acupuncture/ GuideDoc: http://guidedoc.com/chiropractic-treatments-vs-acupuncture-pros-cons Tim Bryan St. Lawrence University '15 Mirror Lake Chiropractic Intern
0 Comments
6/22/2015 4 Comments The Graston Technique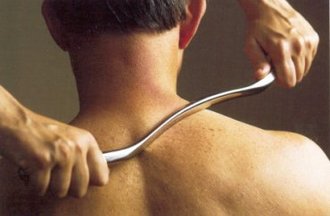 http://www.diversifiedhealth.ca/wp-content/uploads/2011/05/graston.jp http://www.diversifiedhealth.ca/wp-content/uploads/2011/05/graston.jp Since Dr. Gardner often uses the Graston Technique with patients, I thought that I would expand on the topic and provide more information on Graston, how it helps recovery, and what to expect with the treatment. What is the Graston Technique? The Graston Technique is a scientifically advanced from of instrument-assisted soft tissue mobilization that uses specially contoured stainless steel instruments to examine and treat soft tissue injuries. The Graston instruments mobilize, release and lengthen soft tissues that are tight, shortened or restricted, with the end goal being restoration of normal movement and postural alignment. The technique was developed in the early 1990’s and has grown to become popular with chiropractors, physical and occupational therapists and athletic trainers. The Graston approach is used for acute and chronic sprains, repetitive strain injuries and for scars. Injuries such as achilles tendinosis, plantar fasciitis back and neck pain and carpal tunnel syndrome are often treated via application of the Graston Technique. There are six patented Graston instruments that have unique features and contours that are designed to treat different muscles and joints of the body. How Does it Help? The goal of the Graston Technique is to reduce pain levels and increase function of an injured area. Graston treatment involves manipulating the soft tissue with a cross-friction massage with the Graston instrument. The tool is rubbed against the grain of the scar-tissue that has built up due to injury, introducing small amounts of micro-trauma that can sometimes result in inflammation. While it may seem that the Graston Technique causes additional injury, it is theorized that the treatment actually promotes healing to the area through the new micro-trauma. After Graston is applied, the healing process of the body is stimulated, initiating an increase the rate and amount of blood flow, bringing additional oxygen, nutrients and cells that promote healing. What to Expect With Graston Treatment The Graston Technique may cause some discomfort in some patients, depending on their injury and pain tolerance. The cross-friction massage can cause inflammation in the area that is treated and may result in bruising, which is a normal occurrence. The injured area can also be sore after treatment, though the application of ice for 15-20 minutes may ease any potential discomfort. While Graston may cause some temporary discomfort, it has the potential to decrease overall treatment time, result in faster rehabilitation and recovery and reduce the need for anti-inflammatory medicine such as Advil or Aleve. References: Spine Health: http://www.spine-health.com/treatment/chiropractic/graston-technique-indications-and-contraindications Hyde, T. (2007). Conservative management of sports injuries (2nd ed., pp. 300-310). Sudbury, Massachusetts: Jones and Bartlett. Tim Bryan St. Lawrence University '15 Mirror Lake Chiropractic Intern Training for a race that consists of a 2.4 mile swim, a 112 mile bike and a 26.2 mile run presents an athlete with an incredible physical and mental challenge. Unfortunately, triathlon training also provides many opportunities for injury due to cumulative stress and overtraining, which can result in a broad range of injuries. While the potential for injuries may seem daunting to athletes, chiropractic treatment can help to negate these stresses and keep athletes in peak physical condition.
Chiropractic treatment is based on maintaining a homeostasis, or balance, in the body. If the body is out of balance, the body’s mechanics begin to get altered. An imbalance or weakness can cause the recruitment of other muscles or joints in order to compensate. This leads to inefficient bodily movements that can have a negative impact on performance and activities of daily living. Chiropractors attempt to bring the body back into homeostasis by realigning the spine and joints through adjustments and manipulations. Many injuries that are experienced while training for a triathlon can be attributed to a weak core. Improving core and spine stability through chiropractic interventions and adjustments can help to treat current injuries and preemptively treat future ailments by regaining the bodies homeostasis. Chiropractic treatment is also a critical component of recovery after a triathlon. Chiropractic care can help athletes recover by treating injuries to muscles, tendons, ligaments and joints that may have occurred during the race. Post race adjustments to the spine can help to alleviate excess pressure on spinal cord nerves, reducing pain levels across the body. Chiropractic treatment, either in the preparation or recovery phase, is a critical component of triathlon training. References: Princeton Magazine: http://www.princetonmagazine.com/advice-from-chiropractor-and-triathlete-dr-leonard-ershow/ Midland Chiropractic Sports Rehab: http://www.midlandchiropractic.com/runners-and-triathletes-chiropractic-care/ The Joint: http://chiropractorphoenix-thejoint.com/paradise-village/triathlon-pushes-body-to-its-limits-chiropractic-heals/ Tim Bryan St. Lawrence University '15 Mirror Lake Chiropractic Intern  http://wholesaleelectrodes.com/images/1344549048611-375717302.jpeg http://wholesaleelectrodes.com/images/1344549048611-375717302.jpeg What is Electrical Muscle Stimulation? Electrical stimulation treatments involve placing electrodes on the skin over painful or afflicted areas. When activated, the electrodes send small electrical pulses to the muscles below the electrodes, which in turn cause them to become innervated and leads to repeated muscle contractions. While this may sound unpleasant to some, the process is pain free and the contractions often result in a tingling or warming sensation. What are the Benefits of Electrical Muscle Stimulation? One of the main uses of electrical stimulation is for pain relief of the patient. The electrically innervated muscles cause repeated contractions, which leads to an increased amount of blood flow to the area, hastening the healing process. Increasing the blood flow helps to reduce the inflammation around the injury, which also increases the patients' range of motion. Stimulating the muscles can lead to the release of endorphins in the brain as well. These neurotransmitters, the same ones that are released after working out, tend to cause a feeling of euphoria and they enhance immune responses that help to regulate pain. Electrical stimulation can also help to prevent muscle guarding, in which muscles become tense to prevent pain or further injury. The electrical impulses cause the guarding muscles to become fatigued, allowing them to fully relax. Relaxation of the muscles helps to maximize the effects of later treatments. Electrical stimulation can also prevent muscle death and degradation. People with injuries often tend to avoid activities that cause pain or discomfort to the injured area. Doing so can actually lead to muscle degradation when muscles surrounding the injury are not utilized. Muscle contractions via electrical stimulation can help retain muscle mass, tone and strength, even when the surrounding area is injured. Tim Bryan St. Lawrence University '15 Mirror Lake Chiropractic Intern References:
I am often asked what the popping or cracking noise is when adjusting a patient. Patients also wonder why you do not always hear a popping or cracking noise with each adjustment.
To answer, I first want to give a brief explanation of how an adjustment is performed. An adjustment is performed on restricted joints, discovered with palpation. Once the restricted segment or joint is determined the chiropractor can then apply a chiropractic adjustment using a technique that is specific for that joint and also appropriate for the patient. The actual adjustment is a highly controlled procedure, the chiropractor starts with a tissue pull to accurately target a specific joint. Next, a 'lock-out' of the joint must be achieved by bringing the joint to the end of its passive range of motion. Active range of motion is when you use your muscles to move a joint in each direction and passive range of motion is that extra motion that the joint can move if you push it with your hands. It takes years of technique training to learn how to properly bring each joint to the end of passive range of motion. Once the joint is brought to the proper position, the doctor then performs a high velocity low amplitude adjustment. In doing so, the Doctor pushes the joint a short distance past its passive range of motion and as a result, restoring proper motion in the joint. When doing so, there is often a popping or cracking sound, called a cavitation. The noise is actually a collapse of gas bubbles that were in the joint fluid. While the adjustment is being performed, a change in pressure is created within the joint which leads to the release of gas bubbles. The noise is not made from bones, there would have to significant lack of normal anatomy for that to occur! There are a number of structures that separate bony structures within the body including ligament, connective tissue and fluid. Some patients feel it is necessary to hear an audible "pop" in order for the adjustment to be successful. This is not the case, and in fact there is no scientific physiological data that suggests that is necessary in order to restore proper motion in the joint being adjusted. The "pop" or cavitation is just a sound created during the adjustment that a number of patients associate with a successful adjustment and find it satisfying. References: •Spine-health: http://www.spine-health.com/treatment/chiropractic/spinal-manipulation-high-velocity-low-amplitude-hvla •ACA Frequently Asked Questions: https://www.acatoday.org/level3_css.cfm?T1ID=13&T2ID=61&T3ID=152#popping I was asked this week why I do not x-ray all of my patients. A woman asked me, "Well how do you know what's going on if you can't see it?" She went on to explain that her daughter goes to a chiropractor who takes an x-ray of all of his patients and then reviews it with them. This is a great patient education tool and it also allows the doctor to detect conditions that he or she otherwise would not find while performing an examination.
Asking why I do not practice this myself is a great question, there is such diversity within our profession that we are often faced with questions of this nature. I appreciate the diversity within our profession, it proves that we are capable of effectively treating a wide variety of conditions. I answered this woman's question by explaining that if I do not feel that imaging will change my treatment plan then ethically I cannot order the imaging. A detailed history and examination will often give me the information I need to develop an appropriate treatment plan. If it is not needed then I would prefer to treat the patient rather the image. There is also the argument that when unnecessary it is not the standard of care to expose a patient to radiation. Unnecessary imaging also comes with a financial burden, costing billions each year. Reference: Bartoszewski, Melissa DC. "The Clinical Necessity of Imaging". Aug 2014 ACA News. <http://www.acatoday.org/content_css.cfm?CID=5527>. 9/22/2014 1 Comment The Power of the PsoasBrief Anatomy Lesson:
The iliopsoas muscle group is comprised of the psoas major, psoas minor and iliacus. The psoas major muscle attaches to the vertebral bodies and discs of T12 and all of the lumbar vertebrae (L1-L5) and inserts on the lesser trochanter of the femur. The psoas minor is actually absent in 40% of people! When present, it attaches to the vertebrae and discs of T12 and L1 and in some cases to L2 as well. The psoas minor inserts on the pectineal line. The iliacus attaches to the superior 2/3 of the iliac fossa, the iliac crest, and the base of the sacrum and inserts on the tendon of the psoas major and the lesser trochanter of the femur. The action of this muscle group is hip flexion. Why is it Important? Dr. John Stump explains in his paper titled "America's Continued Back Attack", the increased amount of time Americans spend sitting each day and the lack of physical activity are at the root of the problem of back pain and obesity. While sitting, some of your muscles relax and some are overworked, remaining in this position for too long leads to muscle imbalance. The iliopsoas muscles become shortened and tight and can actually lose its functionality. When shortened, the muscle can pull on its attachment site in the low back, leading to low back pain. Travell and Simons have mapped the trigger point pain referral of the psoas muscle and they have found that there are numerous locations in the psoas muscle where trigger points can refer to the low back. The most frequent complaints when a trigger point is present in the psoas muscle are low back and hip pain. The trigger points can be activated by prolonged sitting, driving and sleeping in a fetal position. Treatment To treat the psoas muscle I either have the patient lay in side posture or face up on the table. As the patient takes a deep breath in I will wrap my fingers around the iliac crest (the anterior superior iliac spine more specifically). Once in contact with the muscle, the patient is instructed to slowly straighten their ipsilateral (same side) leg. If tolerable, the patient can slowly internally and externally rotate their hip at that time and then bring hip and knee into flexion to relax the psoas muscle. Once in a relaxed position I once again ask the patient to take a deep breath and I sink my fingers deeper into the muscle and repeat. The location of this muscle deep within the abdominal cavity results in a very different feeling while receiving treatment. It is a very odd but yet relieving feeling. Home Care It is impossible to avoid sitting, as a society we work longer hours at our desk, we have longer commutes sitting our vehicles and we sit down at home after work more than ever before. Incorporating an exercise routine that focuses on strengthening the core and low back will have a long lasting beneficial effect. Additionally, there is a very simple practice that you can incorporate into your daily life that would help break this cycle of muscle shortening and low back pain. The Bruegger's Relief Position is most effective when performed every 30-60 minutes. The position is achieved by sitting at the edge of the chair, with your legs slightly apart and your feet on the floor. The feet and knees should be slightly turned out and the pelvis tilted slightly forward. You should establish a slight “hollowing” of the lower back and increase its curvature (called lordosis). Your chest should be lifted both up and out, which should allow the shoulders to settle backwards without strain. The arms are allowed to rest on the thighs with the hands facing forward. Lastly the chin is gently tucked in and the head high and facing directly forward. Open the pectoral muscles, allow for proper breathing, let the shoulders relax, and focus on gently drawing your shoulder blades down and together. Hold this position for approximately 10 seconds, relax and repeat two more times. References: Stump, John L. "America's Continued Back Attack". June/July 2013 ACA News. <http://www.acatoday.org/content_css.cfm?CID=5202> Dr. Perry, Laura. "Iliopsoas Trigger Points: Hidden Pranksters of Low Back Pain". Jan. 2013 The Trigger Point Therapist. <http://www.triggerpointtherapist.com/blog/psoas-pain/iliopsoas-trigger-points-low-back-pain/> 8/5/2014 0 Comments Simple Lifestyle TipsFor patients recovering from a recent episode of acute back pain, there are a number of practices that you can easily implement into your daily life that will help prevent another episode of back pain.
The American Chiropractic Association publish a list titled "Tips to Prevent Back Pain": •Maintain a healthy diet and weight. •Remain active-under the supervision of your doctor of chiropractic. •Avoid prolonged inactivity or bed rest. •Warm up or stretch before exercising or other physical activities, such as gardening. •Maintain proper posture. •Wear comfortable, low-heeled shoes. •Sleep on a mattress of medium firmness to minimize any curve in your spine. •Lift with your knees, keep the object close to your body, and do not twist when lifting. •Quit smoking, smoking impairs blood flow, resulting in oxygen and nutrient deprivation to spinal tissues. •Work with your doctor of chiropractic to ensure that your computer workstation is ergonomically correct. It is easy to dismiss and forget the importance of wellness practices in our busy lives. If you choose to live by these basic lifestyle tips you may find that you have more energy throughout the day and decreased overall pain and discomfort. Lifestyle changes of this nature have the power to make your body become more resilient. Reference: https://www.acatoday.org/level2_css.cfm?T1ID=13&T2ID=68 |
AuthorMalorie Gardner, D.C. Archives
October 2016
Categories |
Website by North Shore Solutions

 RSS Feed
RSS Feed